What is Insulin Resistance? Can it be reversed?
Insulin resistance occurs when the cells of the muscles, fat, and liver become insensitive or resistant to insulin, causing the body to produce higher insulin levels to compensate in the primary goal to optimize blood glucose and its utilization as fuel. This state of hyperinsulinemia is highly inflammatory for your entire body, especially your arteries and nerves. Eventually insulin production fails and blood sugar levels begin to rise. It is at this point the patient is diagnosed with diabetes based on elevated blood glucose/”sugar”, the final stage of "diabesity."
However, even thin, lean people can be insulin resistant, especially if muscle mass is low (sarcopenia) relative to body fat, especially visceral fat.
In reality, insulin resistance is so common that we should assume its presence till proven absent. Why is it so common to be called a “feature” rather than a “bug”? Why wouldn’t evolutionary pressures get rid of it? The answer: It is a benefit to the hunter gatherer lifestyle. It is not well suited for our current cultural promotion of “grazing” constantly on sweets, starches and highly processed snacking. And, it doesn’t cause death prior to reproduction.
The answer: Eat like a hunter gatherer! Eat within a short time window (6 hours is ideal) and eat lots of vegetables, some fruit (sugary!), meat/protein and good fat (olive, coconut or avocado oil, seeds, nuts).
What is Diabesity?
Diabesity is the spectrum of adverse health effects of diabetes and obesity. It is the result of a modern environment of processed food loaded with sweets and starches consumed throughout the day.
Before rising glucose levels are detected, the higher insulin levels (caused by insulin resistance) raise blood pressure and create inflammation that contributes to arterial injury. We call this injury and the resulting inflammation and scarring atherosclerosis. It can also lead to diabetes, dementia (Type 3 Diabetes?) erectile dysfunction, and depression. Risk of heart attack, stroke, and dementia also increase.
We develop "tolerance" to the toxic effects of sweets and insulin. This leads us to crave more sweets, driving our insulin levels higher, and can lead to early death and disability if unrecognized and untreated.
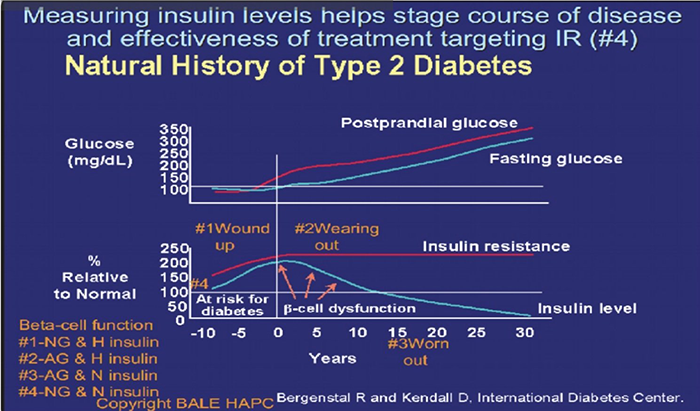
Image Source: International Diabetes Center
This graph illustrates the relationship between insulin resistance, rising insulin levels, and blood glucose levels associated with the progression from insulin resistance (“pre” prediabetes, prediabetes to Type 2 Diabetes. It should be labeled "The Natural History of "Diabesity."
What are some indicators of Insulin Resistance/Diabesity?
Some indicators of insulin resistance include (but are not limited to):
Increased waist size
Elevated visceral fat
High blood pressure
Elevated blood sugar
High triglycerides
Low HDL cholesterol (Metabolic syndrome)
Small dense LDL predominance (Pattern B)
Heart attack or stroke
Gestational diabetes
Polycystic Ovary Syndrome
Erectile Dysfunction
Ananthosis Nigricans
Periodontal disease
How do we identify Insulin Resistance/Diabesity?
The gold standard identifier of insulin resistance includes a two hour oral glucose tolerance test with simultaneous insulin levels. During this test, your blood is drawn before and after drinking a sugary liquid to see how your body responds. Measuring against certain high benchmarks define diabetes and prediabetes. Normal glucose (blood sugar) levels should be below 125 after one hour of this test and 120 after two hours.
Fasting glucose levels above 90 should raise concerns about insulin resistance until other measures are used to rule it out.
Other measures used to identify insulin resistance include: high triglycerides, low high-density lipoprotein (HDL), small and dense low-density lipoprotein (LDL), hypertension, non-alcoholic fatty liver disease (NAFLD), and idiopathic neuropathy.
At the CureCenter, we perform body composition analyses on all of our patients to help identify insulin resistance/diabesity. Elevated visceral fat (which correlates with percent body fat) can be detected in a few minutes, revealing some of the earliest evidence.
Visceral fat can be hard to identify without a body composition analysis, as one may appear “thin” on the outside, but still have high levels of visceral fat. These healthy looking individuals have low muscle mass, known as sarcopenia. This occurs most commonly in women after they experience menopause, especially if they avoid resistance exercises.
New options for continuous glucose monitoring, like Lingo and Stelo make continuous glucose monitoring available without a prescription at affordable pricing for the masses. The feedback, seeing the actual real time impact of food choices and other behavior, make this perhaps the most powerful tool in our battle against cardiometabolic disease.
How do we reverse Insulin Resistance/Diabesity?
Dietary Changes: First, cut out sweets, starches, and snacks from your diet. Excess sugar in your daily diet is stored as fat, worsening insulin resistance. Avoid sugar, artificial sweeteners, processed foods, and white bread, pasta, potatoes, and rice. These all raise insulin levels (even in the absence of high amounts of calories) and perpetuate cravings for sweets. These cravings can lead to food addiction, much like addictions to drugs and alcohol.
In order to effectively reverse insulin resistance/diabesity, be sure to eat more vegetables, protein, and good fats (from sources such as nuts, seeds, and fish).
Although fruit contains important sugar as well as vitamins, eat it in moderation. Fruit is higher in sugar (especially if dried or juiced). Eat whole fruit in limited amounts to ensure healthy glucose levels. Berries are the best. Bananas and grapes are like candy bars and M&Ms!
Exercise: Get off the couch. A sedentary lifestyle is a recipe for all types of chronic disease. While nearly all types of physical activity can be beneficial, we recommend high intensity interval training and/or a focus on building muscle through resistance training in addition to aerobic/cardio exercise.
Restricted Feeding/Fasting: At the CureCenter, we see the best results in individuals who restrict their good food intake to an 8-hour window each day. In the other 16 hours of the day, drink only water or unsweetened beverages.
For additional information about healthy fasting, we recommend resources created by Dr. Jason Fung, including his books, “The Obesity Code,” and “The Diabetes Code,” blog (The Fasting Method), and YouTube channel.
Proper Amounts of Sleep: Poor amount and quality of sleep has been linked to higher levels of insulin resistance. Be sure to get proper amounts of sleep each night. More is generally better. Very few of us get enough sleep. It is rare to get too much sleep in the absence of sleep apnea.
Manage Stress: High levels of stress have also been linked to insulin resistance. Although it’s not always easy, try to find ways to relieve stress to reduce cortisol levels that can raise glucose and insulin. Exercise is a proven and healthy way to reduce stress, so get off the couch and go outdoors or to the gym. Mindfulness practices such as meditation, prayer, or yoga can also help to manage stress.
Measure Your Results: When you first start on your journey to reverse resistance to insulin, it’s best to measure your results every 1-2 weeks by taking a body composition test (these can be done at the CureCenter office). When you’ve met your goal, continue to test every 1-2 months to ensure you are staying on track. Staying accountable is key. Seeing improvement perpetuates the process.
We call it M&M’s (the healthy kind): Measure, Motivate, and Maintain Momentum.
Supplements and Medication (if goals not achieved by lifestyle changes alone ): Sometimes, insulin resistance is so stubborn that a healthy diet and exercise do not achieve the reduction in fat that one may expect. This can be due to an incomplete commitment to carbohydrate restriction or insufficient patience. We cannot out-prescribe a bad diet. However, sometimes a little help is needed. At the CureCenter, we will prescribe medications and/or supplements that best suit your needs and lifestyle.
I’m often asked about metformin. Metformin reduces glucose primarily by reducing release of glucose from liver stores of glycogen, but it is also considered an insulin sensitizer. There is a lot of interest in it as an antiaging and anticancer treatment. Its impact on cardiovascular outcomes is not as impressive as pioglitazone, a thiazolidinedione medication.
Pioglitazone improves insulin sensitivity. It is generic and has been around for a long time. It suffers from a bad reputation for fluid retention because its use was delayed till patients with Type 2 Diabetes had failed 1st line drugs that increased the risk of heart damage from prior heart attacks. But when used in the prediabetes stage, before the damage to the heart, it is well tolerated and dramatically reduces the risk of heart attack (>70% reduction) while lowering insulin levels. See Figure 3: