CureFAQs: Frequently Asked Questions
Answers to commonly asked arterial and metabolic disease questions.
Categories
Click on one of the categories below or type a keyword into the search bar to get started.
Recent FAQs
How can I have a problem? My nutrition and lifestyle are excellent.
If you’re making optimal choices regarding nutrition, exercise, work life balance and supplements–but still not seeing the results you hoped for–consider this...
If you’re making optimal choices regarding nutrition, exercise, work life balance and supplements–but still not seeing the results you hoped for–consider this:
First of all, congratulations!
Your odds of living a higher quality and longer life are far better because of the good choices you make. Without good choices, your results would likely be far worse.
Thank you.
Your efforts benefit not only you, but also your family and your community. By staying healthy and active, you’re able to support others instead of becoming sick, dependent or disabled.
However, hidden risks might still be at play–through no fault or awareness of your own.
Some health threats can hide beneath the surface and are invisible to even the most disciplined individuals. Here are a few:
Genetic Factors:
Epigenetics: Some genes are subject to reduced expression (or can be “turned down”) with specific measures.
Insulin resistance: Even if you are lean and fit, insulin resistance can creep in–especially after menopause or andropause.
Lipoprotein(a): This inherited cholesterol particle increases risk and may respond to treatments like niacin or aspirin.
9p21 Gene Variant: A known risk marker for cardiovascular issues.
MTHFR Gene Mutation: May require more intake of methylated forms of folic acid and B12.
ApoE Genotype: Might call for adjustments in your diet based on your specific genotype.
Haptoglobin Genotype: In some people, gluten is more inflammatory and Vitamin E can do more harm than good.
Even if your ancestors had unhealthy habits and suffered from heart disease or strokes, your genetic “bad luck” might still need more than just good behavior to overcome.
Oral Health Risks:
Periodontal Disease: Dangerous bacteria in the mouth can inflame the gums and the arteries. These bacteria can even be shared through kissing or contact with pets.
Dental Providers Without a Systemic Focus: Complacent oral health providers tend to be focused primarily on traditional dentistry and not on health connections, threats and opportunities for overall optimal health.
Endodontal Conditions (Dental Abscess): Infections like dental abscesses can be asymptomatic for weeks or months, but can still affect your health. These are detectable through blood work or dental imaging. Think: failed root canals, deteriorating crowns or delayed dental treatments due to cost or inconvenience.
COMMON MYTHS & MISLEADING ADVICE
Biased or Dated Guidelines: Mainstream medical advice (like the discredited food pyramid and the misguided obsessive focus on cholesterol) is often based more on politics than proven results. One might wonder if the intent is more, not less, disease as a business model.
Internet “Experts”: Podcasters, pundits and other media may be motivated more by monetization and attention than helping you achieve real, measurable health outcomes. And they can only address generalities, not your specifice circumstances or needs.
Product Pushers: Opportunists may promote products for profit over individual results. Pharma is criticized for its incentives and corruption of regulation. Doesn’t the same risk exist in the less regulated nutraceutical environment? Should it be trusted more or less? Is a friend or family member sharing a benefit or profiting from your purchase and participation in a marketing program?
STAY OPEN-MINDED AND INFORMED
We all have blind spots. Be open to learning new information to enhance the progress you’ve already made. Don’t be offended or take new information or feedback personally–it’s not a criticism of your efforts, but a chance to build on them.
Beware the nocebo effect–the power of negative expectations to produce negative results (a self-fulfilling prophecy).
Treatment decisions should be based on objective, measurable results–not anecdotes, beliefs or assumptions. Biased studies and the experience of others don’t predict personal experience with a supplement or drug.
FINAL THOUGHTS
All recommendations are intended for your personal benefit.
You always have the right to accept or decline any treatment.
Conflicting advice is common–your job is to choose what makes sense for you and track your results.
Let’s work together to make you–and your arteries–as healthy and youthful as possible.
Is genetic testing worth the effort?
Genetic testing should be chosen with an emphasis on tests for which there is a treatment decision that can change the gene expression. Gene expression is the process by which our genes create proteins that perform different functions in our body, such as building and repairing tissues or fighting off infections…
Recommended genetic testing should emphasize tests for which there are meaningful remedies that can change the gene expression. Gene expression is the process by which our genes create proteins that perform different functions in our body, such as building and repairing tissues or fighting off infections.
Genetic testing in low-risk individuals with no plan for lifestyle or treatment changes is expensive, confusing and futile.
What genetic tests are most helpful?
Haptoglobin genotype is very worthwhile, especially those with Type 2 Diabetes, insulin resistance, or prediabetes. Most of us fall into one of these categories!
The cost of this test has decreased significantly over the years. In 2018 the test cost about $400. Now, the cost is $99, a small price for precision in personalized treatment. Because it isn’t offered by Quest or Cleveland Heart Lab, we use Boston Heart Diagnostics and provide you their kit to obtain the proper specimen as close to your home as possible at an affordable cost of $99 out of pocket. It is not covered by insurance, which might tell you the information can actually improve your health and reduce your costs!
How does haptoglobin genotype guide treatment?
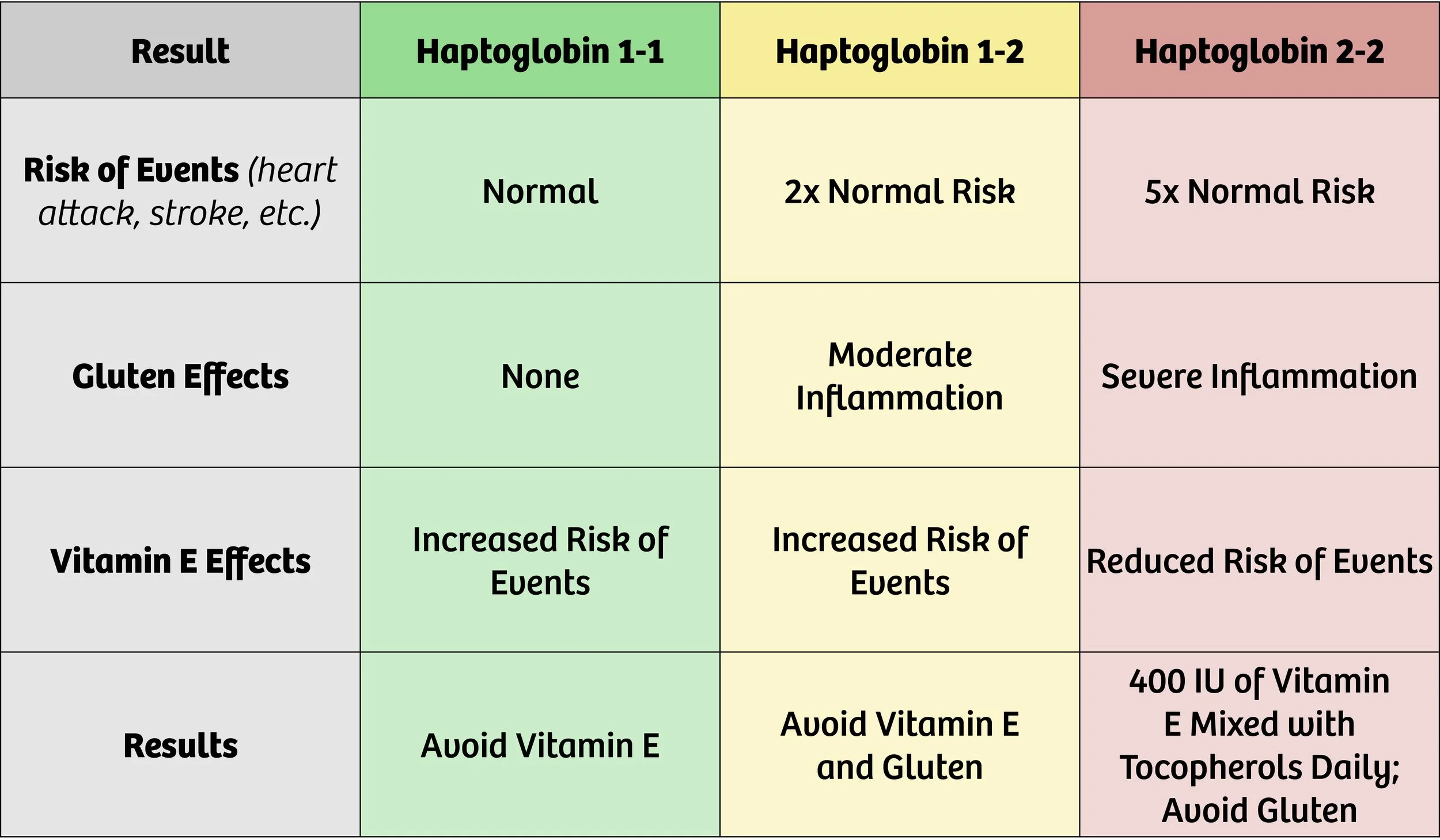
The table below outlines the implications of knowing your haptoglobin genotype.
Haptoglobin Genotype Results and Recommendations
Haptoglobin (Hp) 1-1 is the genotype at the lowest risk for vascular events such as heart attack or stroke. Haptoglobin 1-2 doubles this risk (increases it by 200%). Both of these findings indicate that events are more likely to happen if an individual takes daily vitamin E supplements beyond what is contained in a multivitamin or diet.
Individuals with risk of macular degeneration may be taking supplements containing higher amounts of vitamin E. If your specialist is treating you for current macular degeneration, these supplements make sense. However, you should know that there is a tradeoff. Treating the risk of one condition may increase your risk of another. (See the table above for more information.)
Haptoglobin 2-2 genotype increases risk of vascular events by 500% (or 5x the baseline risk). Gluten should be avoided if this genotype is found, as it provokes a significant increase in inflammation, leading to a higher risk of events.
Individuals with the Haptoglobin 2-2 genotype should take a daily dose of 400 IU of Vitamin E mixed tocopherols to significantly reduce cardiovascular risk by 80%! The proof is greatest in those with Type 2 Diabetes, but most of us have the prediabetic curse that was a blessing when we ate like hunter gatherers.
What is the relevance of ApoE genotype?
We don’t order ApoE routinely, but if you want it, we can order it. In select situations, it can help guide dietary choices, but are less relevant if insulin resistance and carbohydrate restriction is the more compelling opportunity. It often adds more “noise” than “signal.”
The Apolipoprotein E (ApoE) genotype is a genetic factor that plays a significant role in various aspects of human health, particularly in relation to lipid metabolism and the risk of developing certain diseases. The ApoE gene encodes a protein that is involved in the transport and metabolism of lipids, including cholesterol, in the body. There are three common variants or alleles of the ApoE gene: ApoE2, ApoE3, and ApoE4.
The relevance of ApoE genotype lies in its association with several health conditions, including:
Alzheimer's Dementia: The ApoE4 allele is the strongest known genetic risk factor for late-onset Alzheimer's disease (AD). Individuals who inherit one copy of the ApoE4 allele from either parent have an increased risk of developing AD, while those who inherit two copies have an even higher risk. But if you are really interested in reducing your risk of dementia, read “Healthy Heart Healthy Brain” by Bale and Doneen and “The End of Alzheimers” by Dale Bredesen.
Cardiovascular Disease: The ApoE genotype is also linked to the risk of developing cardiovascular diseases such as coronary artery disease and stroke. ApoE4 carriers have been found to have higher levels of LDL cholesterol (often referred to as "bad" cholesterol) and an increased susceptibility to atherosclerosis, a condition characterized by the buildup of plaque in the arteries.
Lipid metabolism: The ApoE genotype influences how the body metabolizes lipids. ApoE2 is associated with lower levels of cholesterol and a reduced risk of cardiovascular disease, while ApoE4 is associated with higher cholesterol levels and an increased risk.
Traumatic brain injury (TBI): Research suggests that the ApoE4 allele may be associated with an increased risk of poorer outcomes following TBI, including a higher likelihood of developing neurodegenerative disorders later in life.
It's important to note that while the ApoE genotype can provide insights into an individual's predisposition to certain conditions, it does not determine with certainty whether someone will develop these diseases. Other genetic and environmental factors generally play a more compelling modifiable role, and individual health outcomes are complex and multifactorial. Genetic testing and counseling can help individuals understand their ApoE genotype and its implications, but it's always best to consult with a healthcare professional for personalized advice and interpretation of genetic information.
What is the relevance of KIF6 genotype?
We rarely order the KIF6 genotype. Our preference for rosuvastatin makes it largely irrelevant to guide treatment. If you insist on using atorvastatin, pravastatin or simvastatin, I suggest verifying this is wise based on KIF6 predicting benefit.
The KIF6 (kinesin-like protein 6) genotype refers to a specific genetic variation in the KIF6 gene. This gene has been studied in relation to cardiovascular health and response to certain medications. However, it is important to note that the current understanding of the relevance of KIF6 genotype is limited, and more research is needed to fully understand its implications.
The KIF6 gene variant in question is known as KIF6 719Arg. It has been associated with an increased risk of coronary artery disease (CAD) and heart attacks in some studies. Individuals who carry this genetic variant may have a higher likelihood of developing these cardiovascular conditions compared to those without the variant.
The KIF6 gene has also been investigated in the context of statin medications, which are commonly prescribed to lower cholesterol levels and reduce the risk of cardiovascular events. Some studies have suggested that individuals with the KIF6 719Arg variant may experience a greater reduction in cardiovascular events when treated with statins compared to those without the variant. However, these findings have not been consistently replicated across all studies.
There is evidence that those with the KIF6 719Arg variant get more benefit from atorvastatin and pravastatin than those not carrying that variant. We prefer rosuvastatin as effective despite genetic variation and less prone to exacerbate insulin resistance/diabetes or cross the blood/brain barrier affecting cognition. Most of our patients take 5 mg 3 days weekly or less with benefit documented with blood and ultrasound inflammation measures.
It's important to understand that genetic factors, including the KIF6 genotype, are just one piece of the puzzle when it comes to cardiovascular health. Other factors such as lifestyle choices (e.g., diet, exercise), family history, and other genetic variations collectively contribute to an individual's risk for developing cardiovascular conditions.
Overall, while the KIF6 genotype has shown some associations with cardiovascular health and response to statin therapy, its clinical utility is still being explored, and further research is needed to determine its exact relevance and potential implications in healthcare practice.
For more information about genetic testing see our post about genes and how they affect your risk of heart attack.
What is lipoprotein A/Lp(a)? Why could it put me at high risk for heart attack and stroke?
Lipoprotein A or Lp(a) is a subtype of LDL cholesterol. The BaleDoneen Method calls Lp(a) the "mass murderer" because elevated levels of Lp(a) triples your risk of heart attack and stroke. At the CureCenter, we call it the “worst” cholesterol…
Lipoprotein A or Lp(a) is a subtype of LDL cholesterol. The BaleDoneen Method calls Lp(a) the "mass murderer" because elevated levels of Lp(a) triples your risk of heart attack and stroke. At the CureCenter, we call it the “worst” or “really bad” cholesterol. Think of it as “highly flammable” lipid.
Elevated Lp(a) affects around 30% of the population, yet it is not included in standard lipid testing. Why?
In the past, the test for Lp(a) was expensive. Today, it only costs about $10 and is becoming more common, yet still not routine. Change in practice tends to be slow, particularly in bureaucratic systems designed to keep revenue flowing through interventions. New drugs and associated revenue are on the horizon, potentially explaining a resurgence in interest.
What causes elevated Lp(a)?
Elevated Lp(a) is a genetically determined root cause with little impact from lifestyle or medications.
Genetics determines Lp(a) levels. You are much more likely to have elevated Lp(a) if you have a family history of high Lp(a).
Why does elevated Lp(a) increase risk for heart attack and stroke?
Lp(a) is made of cholesterol, protein, and fat. Elevated levels (>75 mg/dl) increase the likelihood of development of atherosclerosis, leading to heart attack and stroke. Elevated Lp(a) also increases the risk of calcific aortic stenosis, a valve disease that can lead to heart failure. Finally, it accelerates blood clotting. When atherosclerotic plaque ruptures, a blood clot forms more rapidly to occlude blood flow leading to a stroke or heart attack.
When combined with high levels of inflammation, elevated Lp(a) fuels that inflammation in the artery wall and leads to the formation of plaque.
Lp(a) is not included in standard lipid panels ordered by most doctors. It should be.
While its effect is often lost in the statistics of large population studies, Lipoprotein (a) can be dangerous for the minority with significantly elevated levels. For this reason, everyone should have it measured once, especially if you have:
Family members who have had a heart attack or stroke at an early age
Premature vascular disease in the absence of other usual risk factors
Familial hypercholesterolemia
Family history of elevated Lp(a)
If your Lp(a) is tested and at a normal level, you will not need a repeat test. Your levels will not rise. However, if it is very high, you and your relatives should know, as they could be at high risk as well.
How are elevated levels of Lp(a) treated?
Niacin is the most effective supplement/drug to reduce levels of Lp(a). We have also witnessed response to Bergamot BPF, an effect we have not seen reported in the literature but have observed incidentally. In our experience Bergamot BPF has had a favorable effect that rivals or exceeds niacin in some cases, and it reduces insulin resistance,a highly prevalent root cause of atherosclerosis.
Lifestyle and statins tend to have very little effect on reducing high levels of Lp(a). They can, however reduce inflammation contribution to disease and cardiac events. Therefore, knowing about the increased risk from Lp(a) can motivate more proactive measures to control these other root causes more optimally.
Knowing about the presence of this "mass murderer" in your body will make healthy diet, exercise, and other risk reductions more imperative. Information is empowering. Become aware of Lp(a) - the “worst” or “really bad” cholesterol.
For further reading on Lipoprotein A, we recommend the BaleDoneen website.
Get Started on the Path to a Long and Healthy Life
Participate in a 15-30 minute Zoom or phone call with Dr. Backs. Your questions about process, cost, insurance coverage and expectations will be answered. You will decide together if the CureCenter and a CurePlan are right for you.
Located in Central Illinois? Schedule your 15-minute CureScreen for arterial disease. It’s quick, painless, and is the first step toward preventing the most common cause of death and disability.